Regression of Lumbar Disc Herniation Following Non-surgical Treatment

Knowledge of the natural history of disc herniation with radicular pain is very important for clinicians because it is a common problem causing patients to seek substantial non-operative and operative care. For instance, patients with the same problem like discogenic back pain going to different clinicians will be told different things and receive different care. With many confusing and contradictory concepts out there, this case report aims to convey the better understanding and clinical practices of lumbar disc herniation with radiculopathy.
The existing pathophysiological mechanisms to explain manifestations associated with symptomatic disc diseases may not necessarily accurate and make predictions that often turn out wrong. The North American Spine Society (NASS) (Kreiner et al. 2014) reflected contemporary concepts and involved in translating research evidence into rationale and practice guidelines on the diagnosis and treatment of lumbar disc herniation with radiculopathy. An appropriate application of key guidelines in clinical decision making is fundamental to keeping the professional up to date on current trends and avoiding overtreatment. This case presentation provides an informative example showing the resolution of radicular pain and regression of herniated disc can be obtained from non-surgical treatment. The concept and reality of overtreatment of symptomatic disc herniation is now generally acknowledged.
A 67-year-old male with a one-year history of low back pain complained of sharp, radiating pain that extended down into bilateral buttocks and lateral legs for about 2 months. The patient reported leg weakness to the extent that he required a walking stick to ambulate. Even with ambulatory assistance, he was only able to walk approximately 50 meters before needing to stop because of bilateral buttock and leg pain. He reported no precipitating incident. Prior to seeking chiropractic care, the patient received pain medication (ibuprofen and acetaminophen), mechanical axial traction, rehabilitation exercises and acupuncture without success.
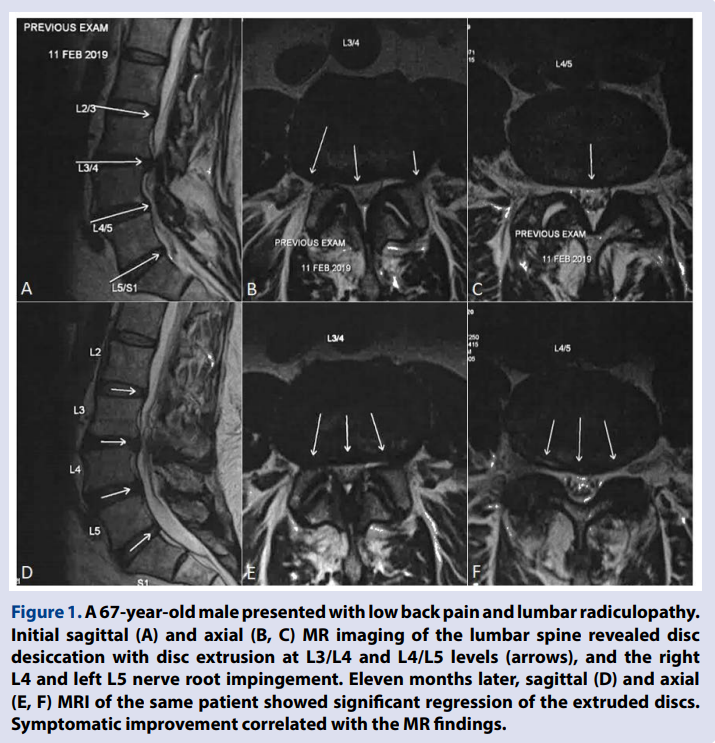
The patient was referred for chiropractic consultation. On physical examination, muscle tenderness was present along bilateral L3-L5 paraspinal regions. The straight leg raise test was negative, while the femoral stretch test was positive bilaterally for increased pain. On neurological examination, his motion strength was reduced in right knee extension (grade 4/5) and left ankle dorsiflexion (grade 3/5). Deep tendon reflexes were normal, +2, with the exception of the right achilles, which was graded +1. Reduced jerk reflex in the right knee and diminished sensation in left lateral leg and dorsal foot were noted. There were no findings for cauda equina syndrome. Lumbar MR imaging (Figure 1A & 1B) revealed lumbar degenerative changes, central and paracentral disc herniation at L3/L4 and L4/L5 levels, and neural compression of right L4 and left L5 nerve roots. A diagnosis of L4 (right) and L5 (left) radiculopathies caused by lumbar disc herniation was made based on the findings of physical and neurologic examinations and MR imaging.
The patient began a regular schedule of chiropractic treatment consisting of thermal ultrasound therapy, lumbar manipulation with a high-velocity, low amplitude force, and skin to skin contact manual adjustment treated daily for 6 days for the first week. A reduced pain score from 7/10 to 3/10 on the Numeric Rating Scale was reported. Subsequent treatment sessions further included an intermittent non-surgical treatment motorized traction (ROBOSPINE Decompression Device, Switzerland) to restore lumbar mobility. Frequency of the treatment sessions was twice weekly for a period of three months and then reduced to once a week for a further 3 months. His pain medication (acetaminophen) was gradually reduced and tapered off near the end of treatment. By the end of 6-month treatment, the patient fully recovered and was able to resume normal daily activities with no residual effects. On his 11-month follow-up, patient reported he had been completely free of symptoms for a period of 5 months. Repeat MRI revealed significant regression of the intervertebral disc extrusions (Figure 1C and 1D).
Knowledge of the natural history of disc herniation with radicular pain is very important for clinicians because it is so very common. For example, patients with a common problem like symptomatic disc herniation going to different clinicians will be told different things and receive different care. As more patients were operated for symptomatic disc herniation, it became obvious that surgery was not universally necessary. The probability of a spontaneous regression was found to be 96% for disc sequestration, 70% for disc extrusion, 41% for disc protrusion, and 13% for disc bulging (Chiu et al. 2015). Bulging of the annulus (much like letting air out of a tire), by definition, is not considered a form of herniation (Fardon et al. 2014). It has been shown that the worse the herniation the more likely it is to completely resolve, namely, the rate of complete resolution of disc herniation was 43% for sequestrated discs and 15% for extruded discs (Chiu et al. 2015).
The conventional understanding is that intervertebral disc herniation occurs when the nucleus pulposus breaks through the ruptured annulus fibrosus. In fact, annular rupture was found in only 35% of patients with lumbar disc herniation (Rajasekaran et al. 2013). In a prospective study of 181 patients who underwent single-level discectomies, Rajasekaran and colleagues observed that the majority (65%) of patients had a failure of the vertebral endplate junction (EPJ), where there was an avulsion in the endplate along with the annulus, rather than a rupture of the disc itself (Rajasekaran et al. 2013). The endplate provides strength and nutrition to the disc and is the weakest portion of vertebral-disc complex, predisposing it to mechanical failure. Moreover, the annulus fibrosus is stronger than endplate junction. Complex loading of compression, torsion or flexion/extension can cause the endplate to fracture before the annulus fibrosus. Previously, the nucleus pulposus has been implicated in pain generation, but now the role of other structures is increasingly being recognized (Sahoo et al. 2017).
Mechanical compression is not the only explanation for the discogenic pain. Recent studies indicate that the structural damages are not necessary in relation to pain. And conversely, symptomatic improvement does not always correlate with radiographic changes of disc regression (Chiu et al. 2015). It is now admitted that interrelated mechanical and biochemical factors are involved in pain generation (Benoist, Boulu & Hayem 2012). Macrophages and other immune cells of the degenerated discs and the herniated materials are able to produce inflammatory mediators (tumor necrosis factors and inflammatory cytokines) which may initiate immune response to the hernia site. The exposure of the nerve roots to irritant substances is responsible for axonal ischemia and nerve root pain (Benoist, Boulu & Hayem 2012; Benson et al. 2010; Cunha et al. 2018). Other than mechanical compression and neurophysiological changes, the pain associated with disc herniation results mainly from inflammatory reactions (Sahoo et al. 2017). Likewise the overwhelming inflammation has also been proposed as a precipitating cause for the regression of the herniated disc.
The mechanism underlying the spontaneous disc regression remains unclear. There are three popular hypotheses proposed to explain the process. The first, a cascade of inflammation, matrix remodeling and angiogenesis (Cunha et al. 2018; Henmi, Sairyo & Nakano 2002), is the most analyzed and convincing hypothesis. It is supposed that the herniated material is recognized by the autoimmune system as a foreign body, which results in enzymatic degradation and macrophage Figure 1. A 67-year-old male presented with low back pain and lumbar radiculopathy. Initial sagittal (A) and axial (B, C) MR imaging of the lumbar spine revealed disc desiccation with disc extrusion at L3/L4 and L4/L5 levels (arrows), and the right L4 and left L5 nerve root impingement. Eleven months later, sagittal (D) and axial (E, F) MRI of the same patient showed significant regression of the extruded discs. Symptomatic improvement correlated with the MR findings. 29 Chun-Pu EC et al., Regression of Lumbar Disc Herniation Following Non-surgical Treatment European Journal of Molecular & Clinical Medicine, Vol 7, Issue 1 phagocytosis triggered by an inflammatory reaction. Ultimately the crosstalk between angiogenesis and inflammation leads to herniated disc regression (Cunha et al. 2018). The second explanation postulates that the herniated disc reduces in size due to gradual dehydration and shrinkage of the nucleus pulposus (Slavin et al. 2001). This supposition may explain the finding that larger fragments regress more than smaller ones, possibly because of larger fragments having more water content. The third is termed the mechanical retraction (Teplick & Haskin 1985). According to an earlier speculation, the herniated material might occur when the pressure of the intervertebral space reduced. This is premised on the fragment has protruded through an annular fissure without separating from it. Nevertheless, it is possible that one specific mechanism or different combinations of the three may operate in spontaneous regression of the herniated disc tissue (Cunha et al. 2018).
The thinking regarding early surgical options for symptomatic disc herniation needs to change due to the favorable natural course of disc herniation. In general, 90% of patients will have improvement of radicular symptoms within 3 months without the necessity of surgery (Donnally, Hanna & Varacallo 2020). As the NASS guideline suggests that the initial treatment for symptomatic disc herniation is medical/ interventional care (Kreiner et al. 2014). Medical/interventional care is a term encompassing pain medication, physiotherapy, exercise therapy, manipulative therapy, local corticosteroid injections, and various types of external stimulators. Either medical/interventional care or surgery appears to be effective for both short- and long-term relief in patients with less severe symptoms. Acupuncture is expected to have the lowest effectiveness of all the conservative treatments (Gadjradj et al. 2017). Surgical treatment is reserved for those with severe symptoms that have failed to respond to medical/interventional care. Systematic studies indicate that early surgery achieves more rapid relief of painful symptoms than conservative care but, in the long run, outcomes gradually become identical to conservative treatment (Jacobs et al. 2011). Patients presenting with red flag symptoms, including spinal fracture, infection, tumor and the cauda equina syndrome, indicate a need for an urgent referral.
This case presentation strengthens the fact that patients with symptomatic disc herniation may undergo symptomatic improvement and that herniated discs appear to have the potential to regress. While we are unable to prove the efficacy of chiropractic treatment alone, the possibility of spontaneous regression cannot be excluded. Additional prospective studies are warranted.